Table of Contents
What is COPD?
COPD is a serious illness that affects millions of people in the United States. COPD is one of the leading causes of death in the United States, affecting over 16 million people in the nation. COPD stands for Chronic Obstructive Pulmonary Disorder and is characterized by increasing breathlessness. There is no cure for COPD, but there are several ways to improve symptoms with medications like Flovent, Pulmicort, and Trelegy Ellipta.
There are many conditions under the umbrella of COPD, but they all can be maintained with proper treatment. With the right doctor supervision, you can achieve a good quality of life and decrease your risk of accompanying illnesses. [1] There are two forms of COPD that patients usually experience, which include:
Chronic Bronchitis: This condition comes with the unpleasant symptoms of coughing and shortness of breath. Chronic bronchitis also comes with a lot of mucus production. There are hair-like fibers (cilia) in your bronchial tubes that help move mucus out of your lungs. Chronic bronchitis occurs when those cilia are lost and you cannot get rid of excess mucus. The excess mucus causes coughing and coughing produces even more mucus. It can become a nasty cycle if there isn’t proper medical intervention.
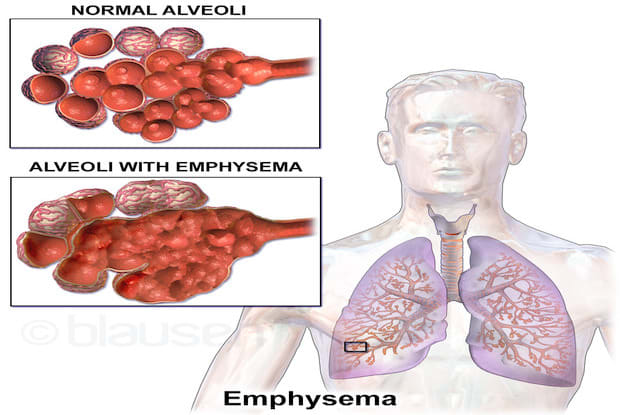
Emphysema: Emphysema occurs when the walls of the air sacs (alveoli) are destroyed and the alveoli merge into one giant air sac. When this occurs, your lungs cannot absorb oxygen as well, so there is less oxygen in your blood. These damaged alveoli can make the lungs stretch out and lose their springiness. People experience shortness of breath when the air gets trapped in the lungs and cannot be expelled properly. Most people with COPD conditions experience a combination of both chronic bronchitis and emphysema. [2] Visit here to learn more about emphysema.
Symptoms of COPD
COPD is a tough condition because symptoms often do not present themselves until there is already significant lung damage. COPD symptoms are more severe if you smoke or are exposed to second-hand smoke. The number one symptom involves a daily cough that produces mucus. This cough and mucus usually occurs for at least three months and upwards of two years. Some common symptoms of COPD include:
- Shortness of breath
- Chest tightness
- Lack of energy
- Unintended weight loss
- Swelling in ankles
- Chronic cough
If you have COPD, you can experience flare-ups, which is when your symptoms worsen during different times. There can be day to day variations of symptoms and it is best to avoid activities that exacerbate your COPD. Visit here to learn more about the risk factors of COPD. [3]
Tests for COPD
There are many ways to test for COPD and it is often misdiagnosed for other lung disorders. A patient usually has to undergo several tests in order for COPD to be correctly diagnosed. Your doctor will examine your signs and symptoms and give you the tests that are right for you. Tests for COPD can include:
Lung (pulmonary) function tests: Pulmonary function tests measure the amount of air that your body can inhale and exhale. These tests help determine how well your lungs are delivering oxygen to the blood. Spirometry tests are most common and include blowing into a large tube that is connected to a small machine called a spirometer.
Once you blow into this tube, the machine will measure how much air your lungs can hold and how fast you can blow the air out of your lungs. This test can help detect COPD even before you have symptoms of the disease. Spirometry tests can be taken several times to track the progression of your COPD. These tests can also help determine how well your medications are working.
Lab tests: Lab tests cannot diagnose COPD, but they can help determine the cause of your symptoms and rule out other illnesses. COPD can be genetic and these lab tests can detect a disorder called alpha-1-antitrypsin (AAt) deficiency, which is a common cause of some COPD cases. If you have a family history of COPD, this test can help with early detection, especially if family members have developed COPD at a young age (under 45). [4]
Arterial blood gas analysis: Arterial blood gas tests usually occur in the hospital if you’re having serious lung problems and trouble breathing. During an arterial blood gas test, a doctor will use a small needle to take a sample of blood from your wrist or an artery in your groin. Results of this blood test will be available quickly and show:
- If you are getting enough oxygen
- Your lungs are removing enough carbon dioxide
- Your kidneys are working properly
Arterial blood gas tests do not singularly determine COPD, so other tests will also be needed to make an accurate diagnosis. [5]
CT Scan: A chest computed tomography scan (CT) is performed to help diagnose COPD or determine its severity. These scans combine x-ray equipment with computers to produce multiple images of the inside of the lungs. These images can help determine COPD and determine the right course of treatment.
Chest x-ray: This test also produces images of the lungs to help determine the cause of a patient’s shortness of breath or chronic cough. Chest x-rays may not show COPD until it is severe, but it can show enlarged lungs, air pockets, or a flattened diaphragm. [4]
Medications for COPD
COPD can affect every aspect of your life and it is important that each patient receives proper treatment for their unique case. Some common medications for COPD include:
Short-acting bronchodilators: These medications relax the muscles of the airways and ease symptoms of coughing and shortness of breath. These medications are most typically taken through an inhaler. These drugs work anywhere from 4 to 6 hours and are used when you have symptoms or before exercise. Some frequently used short-acting bronchodilators include Ventolin and Levalbuterol. These drugs are fast-acting and relieve symptoms quickly. Short-acting, or rescue inhalers, are helpful in a pinch, but they are often paired with a long term inhaler to better control symptoms.
Some side effects of short-acting inhalers can include:
- Dry mouth
- Headaches
- Constipation
- Muscle cramps
- Shaking

Long-acting bronchodilators: These inhalers also relax the muscles around the airways. These inhalers can work for up to 12 hours and are used every day to prevent symptoms. Some common long-acting bronchodilators include Brovana and Serevent.
Some side effects of these drugs can include:
- Constipation
- Dry mouth
- Muscle cramps
- Shaking
- Fast heartbeat
Steroids: Steroids bring down the swelling in your airways. These drugs help with COPD symptoms and flare-ups. Inhaled steroids can take several hours to take effect and doses vary from person to person. For best results, these steroids should be taken daily. Best results are seen after three months of daily use. Some common inhaled steroids include Flovent, Pulmicort, and Trelegy Ellipta. These steroids can come in metered-dose inhalers, dry powder inhalers, and nebulizer solutions.
Steroids reduce the frequency of asthma attacks and improve lung function. Proper use of steroids can also reduce the frequency of emergency room visits and hospitalizations for lung issues.
There are fewer side effects of inhaled steroids, especially at lower doses. You usually have to wash out your mouth after inhaling the medication to prevent thrush (yeast infection in the mouth). Hoarseness of the throat may also occur. [6]

How to improve your COPD
COPD may not be curable, but there are several ways to improve your quality of life and reduce painful symptoms. It is encouraged to seek the help of a dietician to create a meal plan that can reduce COPD flare-ups. Drinking plenty of water is always a good thing, but for those with COPD, it can significantly reduce symptoms. Drinking water helps prevent gas when eating high-fiber food. It also thins the mucus in the lungs which makes it easier to cough up. Some other tips for improving COPD include:
- Avoid smoking/smoke
- Avoid salt
- Avoid foods that cause gas or bloating
- Avoid junk food
- Walk or do light exercises
- Stay up to date on vaccines and flu shots [7]
Visit here to learn more about life with COPD and ways to improve your lifestyle while living with this condition.
The content provided in this article is based on thorough research and in some cases, reviewed by a medical professional. Our goal for the information is to provide helpful, general health informational. It is not intended as a substitute for professional medical advice.
