Table of Contents
I. The Importance of Bone Health
II. What is the Cause of Osteoporosis?
The Importance of Bone Health
Bones play a vital role in the body. Many people may think that organs and other bodily functions are more important, but bones are the structure that keeps our bodies upright. Bones help anchor muscles, store calcium, and protect organs. Our bones continuously change as we grow older. During youth, bones regenerate faster, but this slows down steadily as we age. In general, people reach their peak bone mass around the age of 30. After that, you start to lose slightly more bone than you create.[1]
If you do not have strong bones as a young person, it can have severe side effects as you get older. You typically do not know your bones are weakening until you experience a breakage. If you break bones easily, your doctor may diagnose you with osteoporosis. Osteoporosis is a bone disease that occurs when the body loses too much bone and doesn’t replenish it as quickly as it should. Too little bone regeneration can result in weak, porous, and brittle bones. If you reach peak bone mass later in life, the less likely you are to experience osteoporosis. [2]
When viewed under a microscope, healthy bones typically look like a honeycomb, but if the bone weakens and becomes porous, the honeycomb's holes and spaces become much larger. These large spaces make you more susceptible to bone breakages. This is a fairly common condition, and there are several medications like Fosamax, Actonel, and Boniva available to combat osteoporosis symptoms. Read on to learn more about symptoms, risk factors, and treatment for osteoporosis. [2]
Several factors can cause osteoporosis. Everything from your age, lifestyle, medical conditions, and medications can affect your bone's health. According to the European Journal of Rheumatology, over 200 million people worldwide have osteoporosis. This bone disorder can occur in anyone, but it is most common in menopausal and post-menopausal women. The International Osteoporosis Foundation has found that 1 in 3 women over 50 years old and 1 in 5 men will experience osteoporotic fractures. [3] The most common risk factors of osteoporosis include: Race and Family History: Scientists have found that those who are white or of Asian descent are more susceptible to osteoporosis. This condition can be hereditary, so if you have a close family member with osteoporosis, you will be more likely to experience it. Hormone Levels: Hormones play an integral role in bone health. Too much thyroid hormone can cause bone loss as well as a lack of estrogen production. Estrogen levels in women dip after menopause, which affects the production and rigidity of bones. In men, lower testosterone in older adulthood can also cause osteoporosis. [1] Medical Conditions: If a person suffers from anorexia or bulimia, they are more likely to develop osteoporosis. When a woman’s body weight is low, menstrual periods may stop and lead to a dip in estrogen levels. This will lower your bone density and increase your risk of fractures. Conditions that affect the body’s ability to absorb calcium can also increase your chance of bone breakages. These conditions include Crohn’s disease, stomach surgery (gastrectomy), celiac disease, and Cushing’s disease. Diet and Exercise: Bones rely heavily on the absorption of calcium to maintain strength and rigidity. A lack of calcium can contribute to diminished bone density and lead to fractures. It is also essential to maintain physical activity, and those who remain inactive are at a higher risk of osteoporosis.[1] Medications: Researchers have found the long-term use of corticosteroid medications like prednisone, prednisolone, cortisone, and dexamethasone can damage the bone over time. Other medications used to treat breast cancers and anti-seizure medications, like Dilantin and proton pump inhibitors, can increase your risk of osteoporosis. As mentioned earlier, it is difficult to diagnose osteoporosis before a bone break occurs. The symptoms of this bone disease may be challenging to notice, but it is important to pay attention to any changes in your body. If you are experiencing any of the following symptoms, it is essential to see your doctor and get a bone density test. Even if you do not experience these symptoms, it is smart to regularly see your doctor if you took corticosteroids for a long period or went through early menopause. If your parents suffer from hip fractures, you may want to stay in touch with your doctor so you can keep an eye on your bone density. [4] Because osteoporosis typically has undetectable symptoms, it is essential people take the proper steps to make sure they maintain good bone health. If you are concerned with your bones, your doctor will perform a bone mineral density (BMD) test. A bone density test uses a machine to measure bone density primarily in the bone in the hip, spine, and other commonly fractured areas. It can help detect your risk factor for bone breakages. Doctors recommend a bone density test if you are a post-menopausal woman over 50 years old and have recently broken a bone. This test can help determine: There are two main types of bone density tests, which include: Central DXA: A central DXA machine stands for dual-energy x-ray absorptiometry. When testing cannot be done on the hip and spine, a central DXA test can be done on the radius bone and forearm. These tests usually take less than 15 minutes and require no needles or instruments placed through or on the body. The central DXA also uses little radiation. Screening Tests: These tests measure the bone density in the wrist, finger, lower arm, and heel. The tests used include pDXa (peripheral dual-energy x-ray absorptiometry), QUS (quantitative ultrasound), and pQCT (peripheral quantitative computed tomography). These screening tests are used when central DXA is not available. These tests are especially helpful for those over 300 pounds because people of larger sizes cannot use most central DXA machines. [5] Bisphosphonates are the most common medications used in the treatment of osteoporosis. The types of bisphosphonates include alendronate (Fosamax), ibandronate (Boniva), and risedronate (Actonel). These drugs work by preventing the loss of bone density. One common side effect of bisphosphonates is an upset stomach. These drugs are sometimes available in quarterly or yearly infusions like the Boniva Injection, which some people prefer to a daily pill. Osteoporosis is more common in post-menopausal women, so hormone therapies may also be needed. Estrogen levels in women dip after menopause, so you may need to take estrogen supplements if your osteoporosis is related to a hormone imbalance. Evista (raloxifene) can be used for estrogen-related osteoporosis. The goal of osteoporosis treatment is to slow the breakdown of bones. Osteoporosis medications are typically taken for long periods, especially if you are at high risk for fractures. [6] The content in this article is intended for informational purposes only. This website does not provide medical advice. In all circumstances, you should always seek the advice of your physician and/or other qualified health professionals(s) for drug, medical condition, or treatment advice. The content provided on this website is not a substitute for professional medical advice, diagnosis, or treatment. The content provided in this article is based on thorough research and in some cases, reviewed by a medical professional. Our goal for the information is to provide helpful, general health informational. It is not intended as a substitute for professional medical advice.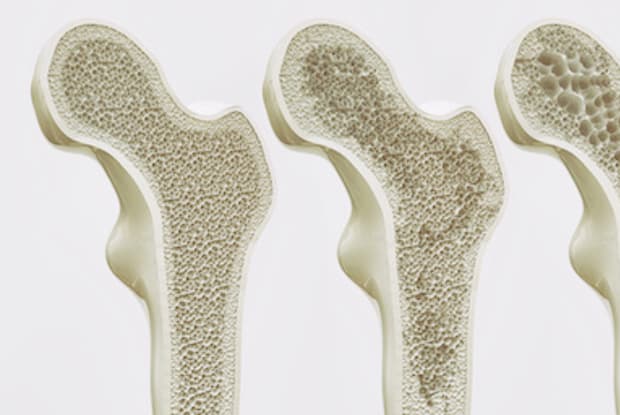
What is the Cause of Osteoporosis?

Symptoms of Osteoporosis

Diagnosing Osteoporosis

Treatment
